Patient is a 67 year old female with a history of pharmacologically controlled hypertension and hypothyroidism.
Tooth #14 was removed approximately 6 months previously due to the presence of pain and a firm buccal alveolar swelling of 2 month duration. Due to the anatomic position of the zygomatic process in this patient, plain radiography was of minimal diagnostic value. Cone beam CT confirmed periradicular pathology. Root fracture was suspected preoperatively and was confirmed the day of tooth removal.
The large defect was grafted with mineralized particulate allograft using a guided bone regeneration technique.
The large defect was grafted with mineralized particulate allograft using a guided bone regeneration technique.
Patient was treatment planned for a dental implant at site #14 with a closed sinus lift after a 6 month healing period.
Tooth #13 is treatment planned for a new restoration.
__________________________________________________________
__________________________________________________________
Preoperative coronal cone beam image of tooth #14 demonstrating a large well contained periapical lesion along the floor of the maxillary sinus.
6 month postoperative periapical radiograph illustrating the appearance of the grafted area.
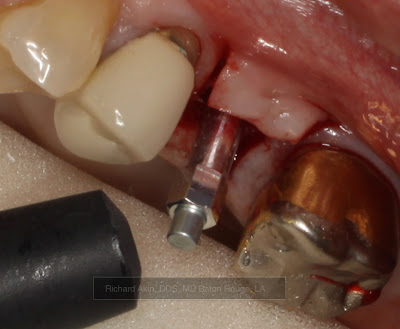
At surgery, bone was noted to be dense (D1).
Final sinus lift osteotome used to depth (~13mm).
4.7mm x 11.5mm Zimmer Trabecular Metal Implant.
Implant insertion torque value was greater than 35 Ncm.
Osstell reading was taken to determine implant stability.
Osstell ISQ implant stability value was 75 at insertion.
(For reference, implants that are ready for final restoration will typically have an ISQ value of 65 or greater.)
Implant at final depth.
Palatal tissue was contoured to accept healing abutment using a rotary tissue punch.